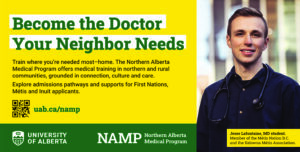
Sponsored by the University of Alberta
(Alberta) – This August, a new generation of doctors will start their medical education closer to home, culture and community.
Thanks to a new partnership between the University of Alberta and Northwestern Polytechnic, medical students can now take all of their training — both classroom and clinical — in Grande Prairie and surrounding northern Alberta communities. Instead of requiring them to move to Edmonton or Calgary, this program will allow future doctors to train in the communities that need them most.
Beginning in the fall of 2025, the Northern Alberta Medical Program will provide 30 spots for students to learn the realities of medicine in rural and Indigenous communities. Program director Richard Martin says these experiences will set future doctors and their patients up for success.
 “It’s so important that people learn in the spaces where they’re needed to practice,” he explains. “[These communities] are only an abstraction when you aren’t there. For the people who are there, this is the reality of life, so it’s very important that everybody has a better grounding in those realities.”
“It’s so important that people learn in the spaces where they’re needed to practice,” he explains. “[These communities] are only an abstraction when you aren’t there. For the people who are there, this is the reality of life, so it’s very important that everybody has a better grounding in those realities.”
Those realities include not only the way care is delivered in rural areas, but also the cultural contexts that come with serving Indigenous communities.
“This puts us in a very unique situation where we’re in a rural and regional part of Alberta and we have very close proximity to nations,” explains Wayne Inuglak Clark. Clark is the executive director of the Wâpanachakos Indigenous Health Program at the University of Alberta, which supports Indigenous medical and dental students.
Clark highlights that students will experience firsthand how the health-care service model looks different for Indigenous communities and nations, especially when compared with urban sites.
“This program offers a new vantage point to deliver culturally safe and community-informed physician training,” he says.“Health-care providers will have a lot more knowledge of Indigenous cultures because it’s more present than in big-city hospitals.”
The University of Alberta collaborated with local and Indigenous communities before the program launch to ensure that the education doctors receive reflects the people they will serve.
“We’ve engaged the community on how we’re going to do this right at the beginning,” says Clark. “They’ve told us what they want and we’re not setting it up and then saying, ‘Does this work for you?’ We’ve involved them in the whole process.”
While the medical curriculum is the same as in Edmonton, this northern program provides new learning opportunities such as land-based learning, as well as Elders and Knowledge Keepers being involved with the program from its foundation.
Although the U of A has existing support systems for Indigenous applicants and students in Edmonton, Martin and Clark both hope that providing a complete medical education closer to home and closer to students’ support networks encourages more Indigenous people to consider becoming doctors.
“One of the strong benefits of taking medical education and distributing it into other places is that it helps to open the door for people from those spaces who might not have imagined being a doctor as a career, and makes it feel more reachable,” says Martin. “They can go through the process much better supported because they’re just closer to their people, their land and everything else that is their foundation.”
“[Students] will be closest to the land that they know, and if they can have their education as much as possible in that same land, the chance that they go back to practising in High Level or someplace very similar is much higher.”
Martin, who has worked in rural family medicine for his entire career, says that context allowed him to become deeply integrated into his community more than he might have been in an urban setting. Rural communities gave him the chance to practice medicine from cradle to end-of-life, all while keeping relationships at the centre of care.
“When I went through medical school, I had a hard time choosing between all of the different things you could do,” he says. “I knew at that time that my choice had to be family medicine because then I could do everything. I did surgery. I delivered babies. I worked in the emergency department. I took care of patients in their care facilities. I love the different places where I can provide care. I love the different types of things that I do. And quite frankly, I just love taking care of people.”
“That relationship building, with patients and their families and my colleagues, was really important to me.”
Both Martin and Clark hope the Northern Alberta Medical Program makes medical education more accessible for students from rural and Indigenous communities and educates the next generation of doctors to be deeply grounded in culture, relationship and community.
They encourage potential students to reach out to the Wâpanachakos Indigenous Health Program before applying to learn more about the supports available to them.


Be the first to comment on "New medical program will train doctors in Northern and Indigenous communities"